Killing a patient: The question divides nurses. While an end-of-life bill promised by Emmanuel Macron is still awaited, The world interviewed around ten doctors, a psychologist and a nurse. Each of them tells of his practice, his relationships with patients, the personal trials he endured and the reasons why he made a deadly gesture – or not. Some say they have already done it.
These supervisors position themselves at a certain point in time: a copy of the bill is currently on the head of state’s desk The world was able to view a version from the beginning of October, provided access to a “Euthanasia”the act is “Basically carried out by the person themselves”. It is also mentioned whether the person is physically unable to do so “Administer the substance yourself”the intervention of a doctor, nurse or even a loved one.
A large part of the nurses who have gathered around the French Society for Support and Palliative Care (SFAP) in recent months have argued this “Death cannot be a treatment” Other White coats consider this gesture as “ultimate care”. Without attempting to measure the balance of power, here are testimonials that allow the question to be examined at the practitioner level.

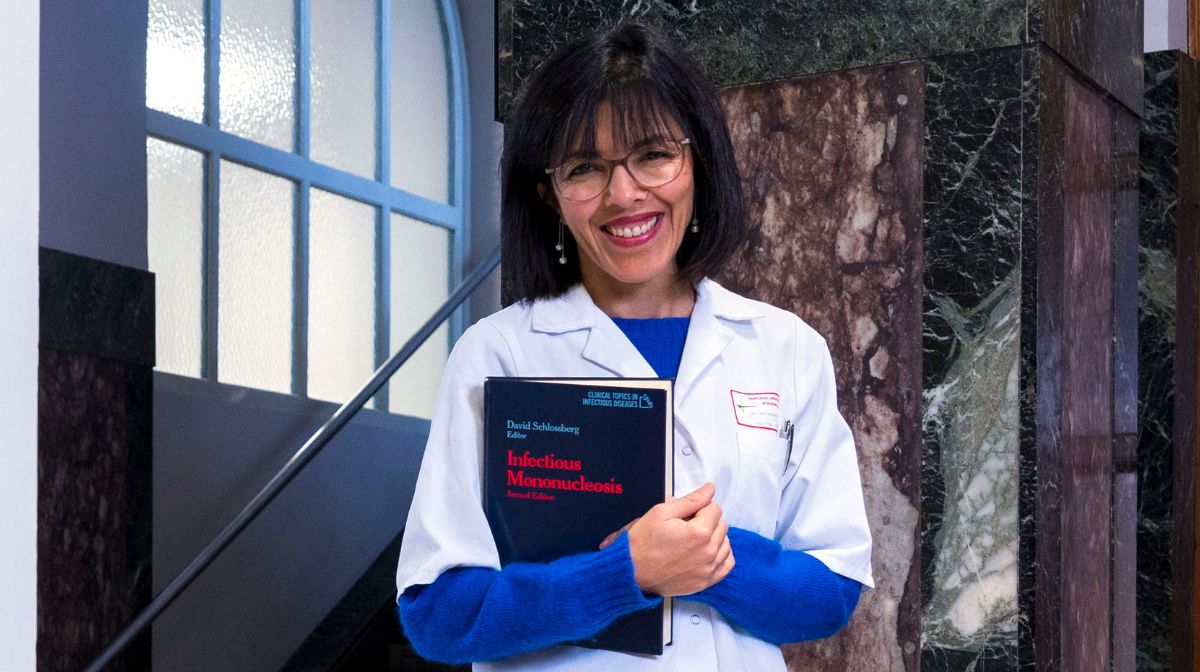
“I was there when she closed her eyes.” remembers the neurologist Valérie Mesnage, who put Ingrid R. fast asleep until her death in 2018 in the Saint-Antoine hospital Paris. The patient suffered from Parkinson’s disease, which made it impossible for her to eat alone, as the patient had reiterated to the doctor “Straight in the eyes” her “ask to end it”.
Since 2016, every patient has been able to – according to the Claeys-Leonetti law – has the “right” a “deep and continuous sedation until death”. Granted, if doctors believe the person is at the end of their life, it is performed when the pain is considered unbearable. Ingrid R.’s ordeal lasted three days. At the end of other sedations carried out, Valérie Mesnage remembers “agonal phases” six or even seven days. “ What is the significance of this period of survival, sometimes unbearable for the relatives, difficult to endure for the medical team? “, asks this Parkinson’s specialist who welcomes us in the attic of the Cochin Hospital in Paris. The sick must be able, she says, “Choosing a different end to life”.
The ordeal of a cousin who died of bone cancer at the age of 30“inhuman” The pain left a deep impression on her. A form of helplessness or even indifference towards the medical profession “Unbearable suffering” the young doctor of the same age said indignantly. His indignation remained unabated. Valérie Mesnage was determined to change the law and initiated it a column published in The world September 8thsigned by a hundred or so supervisors, including several quoted in this article. Euthanasia would be, she continues, “very humanly complicated”. But putting a patient to sleep until he dies, what else is there? “Psychological euthanasia because the patient is finally cut off from his relationship to the world? The difference is that we let fate decide our biological death.” In any case, the doctor decides whether “Switch”. “And this moment is difficult. »
You still have 85% of this article left to read. The rest is reserved for subscribers.