Small vesicles produced by adipose tissue appear to be stable transport vehicles for adiponectin, a hormone that plays a key role in glucose metabolism. Researchers from the Thorax Institute in Nantes, in collaboration with the University of Angers, have just described this. They now want to develop the production of similar vesicles for use as a biomedicine to treat insulin resistance and diabetes.
Adiponectin, a hormone synthesized by cells fatty tissue, improves insulin sensitivity, which is the body’s ability to store glucose for later use. In overweight and obese people, the production of this hormone decreases, which promotes the occurrence of obesity Insulin resistance then one Type 2 diabetes, metabolic disease that is associated with numerous complications. Therefore, administering adiponectin-based treatment could help reduce the risk of diabetes. However, this approach is difficult to achieve. In fact, before they are biologically active, the adiponectin molecules circulating freely in the blood must assemble in groups of three to form trimers, which then assemble into larger complexes: a synthetic process that has proven to be as difficult to reproduce in the laboratory as it was previously expensive, making the clinical one development of this strategy. However, thanks to recent work by Soazig Le Lay and his team, a new approach appears to be emerging: using bioactive forms of the hormone transported by extracellular vesicles (EVs).
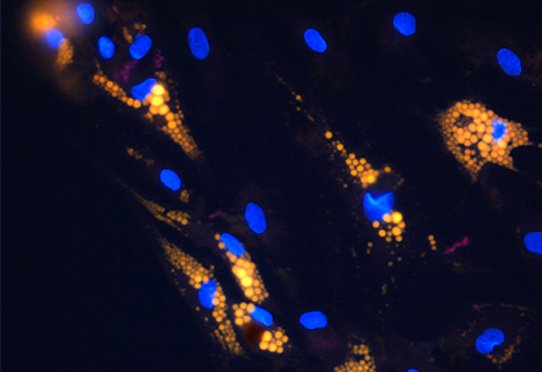
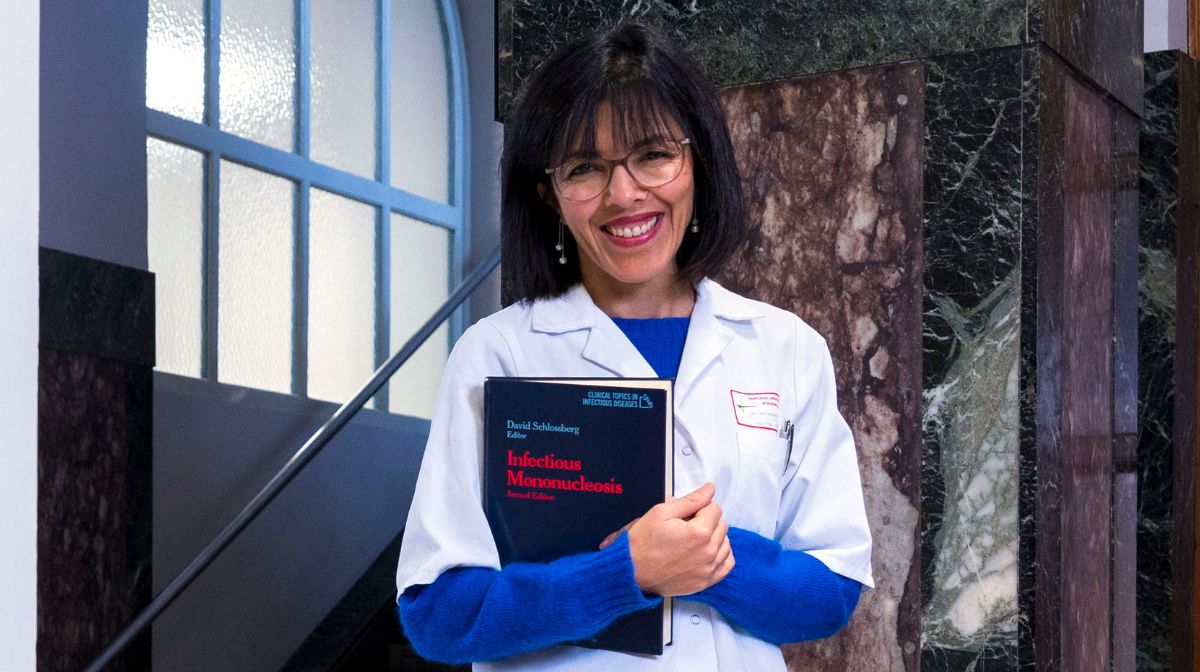
This team has long been working to decipher the nature of the dialogue between organs in cardiovascular disease and is therefore interested in extracellular vesicles: “ These natural nanoparticles are important vectors for intercellular communication in the body. All tissues produce it, including fatty tissue. Their content is specific to the tissue from which they originate, but the bioactive compounds included in the composition of the compounds produced by adipose tissue are not precisely known. », explains Soazig Le Lay. A gap that she wanted to fill in order to assess whether changes in their usual content could be linked to the emergence of insulin resistance or diabetes.
To do this, the Inserm researcher first examined the composition of the extracellular vesicles secreted by the fatty tissue of normal-weight mice: it turned out that adiponectin was one of the most frequently occurring messenger substances. Thus, 20% of its total blood volume would be on the surface or inside these nanovesicles,” “ This shows that adiponectin does not only circulate in the blood in free form », comments Soazig Le Lay. By repeating these measurements in obese mice, the scientists found that the adiponectin content of extracellular vesicles was significantly reduced.
First perspective of insulin sensitizing treatment
To ensure that the vesicular forms of the hormone have the same properties as the free form, the team also conducted experiments to examine their ability to restore insulin sensitivity to cells that have become resistant in vitro Thein vivoResearchers have shown that adiponectin-rich vesicle-based treatment can effectively correct insulin resistance in liver cells. In vivo In mice fed a high-fat diet, the same treatment prevented the development of type 2 diabetes. The team also described that adiponectin limits inflammation, which is known to play a role in triggering or exacerbating metabolic and cardiovascular disorders.
This work therefore confirms that extracellular vesicles are “molecular taxis” of bioactive adiponectin and that this vesicular form – which appears to be more stable than soluble adiponectin – indeed plays an insulin-sensitizing role. Apparently Soazig Le Lay doesn’t want to stop there: “ We received two grants, one from the National Research Agency (Project). Evadipo) and the other from the French-speaking Foundation for Diabetes Research, to develop a treatment based on the use of these adiponectin-enriched vesicles. We have already partnered with a company that has developed a technology for the standardized production of such vesicles from human cell cultures. But of course we are only at the beginning of the process and still need to validate the safety of use and clinical effectiveness of this potential biomedicine. »
This approach gives real hope: there is currently no drug that can restore tissue sensitivity to insulin. The available treatments for insulin resistance act either through direct insulin delivery or on glucose metabolism. If the work developed by Soazig Le Lay’s team is successful, it would represent real progress in the care of patients whose diabetes is poorly controlled with current medications.
Soazig Le Lay is coordinator of the research axis Extracellular vesicles and interorgan communication in cardiometabolic diseaseswithin the Cardiometabolic Diseases Team of the Thorax Institute (Department 1087). Insert/CNRS/University of Nantes, Nantes University Hospital).
source : A Blandin et al. Extracellular vesicles are carriers of adiponectin with insulin-sensitizing and anti-inflammatory properties. Cell Reports, online edition of August 20, 2023; doi:10.1016/j.celrep.2023.112866
Author: CG
also read