To accelerate the healing of chronic or acute wounds that do not heal naturally, scientists from Inserm and Besançon University Hospital are developing a biomaterial that replicates the architecture and physical properties of human skin. When it is transplanted into the patient, it promotes tissue regeneration.
A report in the magazineInsert #58
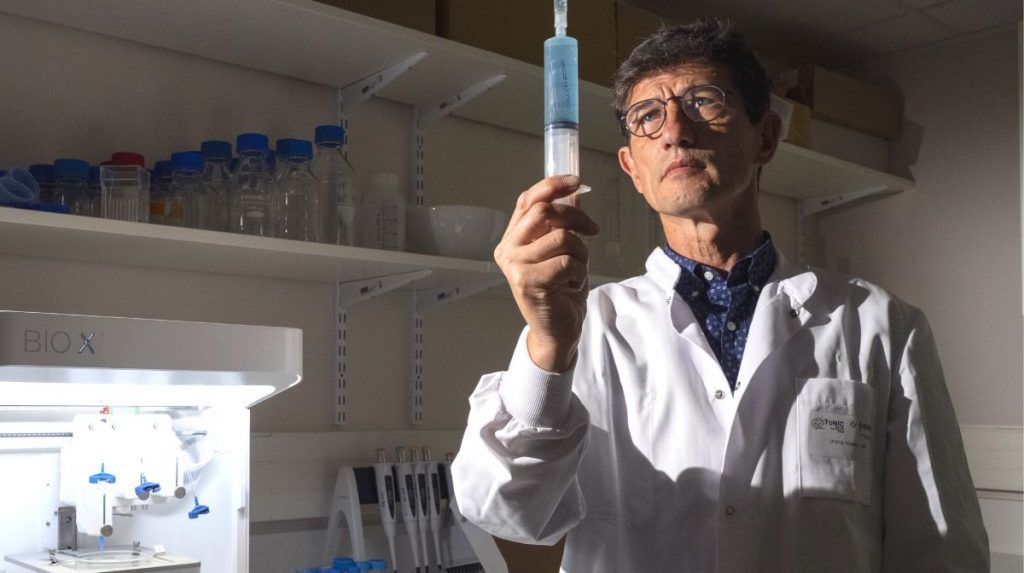
We are located in the heart of the Besançon health campus. The first autumn leaves are already covering the ground walked by the busy students. Researcher Gwenaël Rolin welcomes us with enthusiasm in his laboratory. Today we will test together the TissYou project that he has been developing for ten years: a biomaterial that can regenerate the skin. A type of intradermal dressing that accelerates the healing of chronic or acute wounds. How ? “ The biomaterial is grafted onto the patient’s wound so that his own cells colonize on it and regenerate the skin. As healing progresses, it breaks down before disappearing completely. », explains the researcher enthusiastically. To be effective, the biomaterial must be flexible like human skin and conform to the patient’s skin cells. We will therefore review its mechanical and biological properties. Gwenaël Rolin invites us to follow him into the first room of the laboratory: the demonstration can begin.
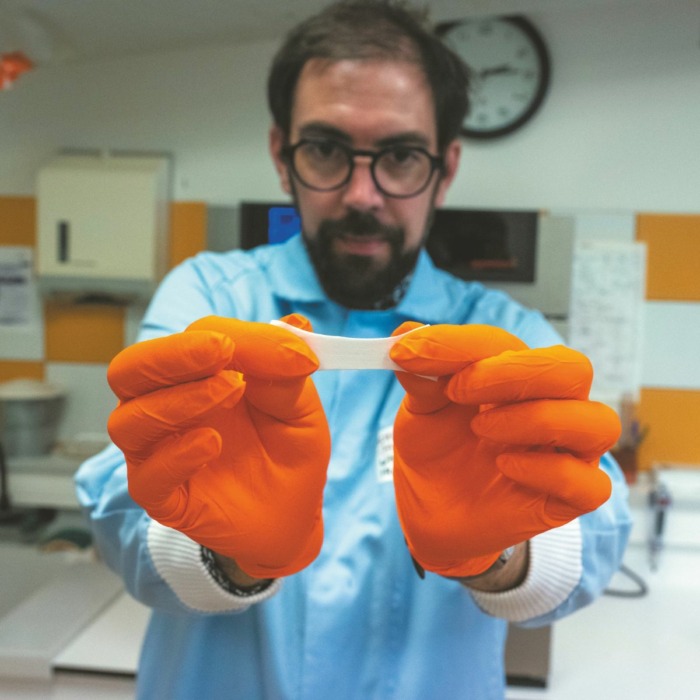
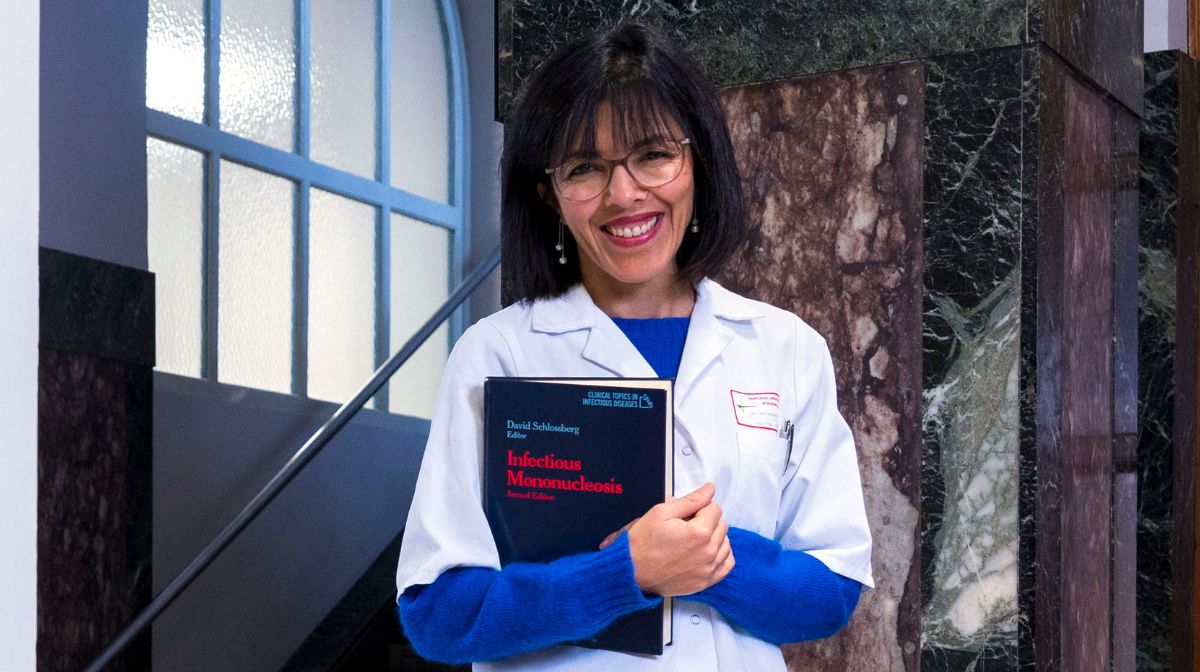
This is what the biomaterial looks like. White, like the deep human dermis, has the same architecture. Slightly elastic, like skin. Gwenaël Rolin is preparing to carry out the colonization of skin cells in the biomaterial in front of us, as if it were deposited in a patient’s wound.
To do this, we first have to obtain cells from human skin donations. These cells, concentrated in the test tube, are individually sorted and characterized. This is called the technique of “ Flow cytometry », here produced by doctoral student Zélie Dirand.


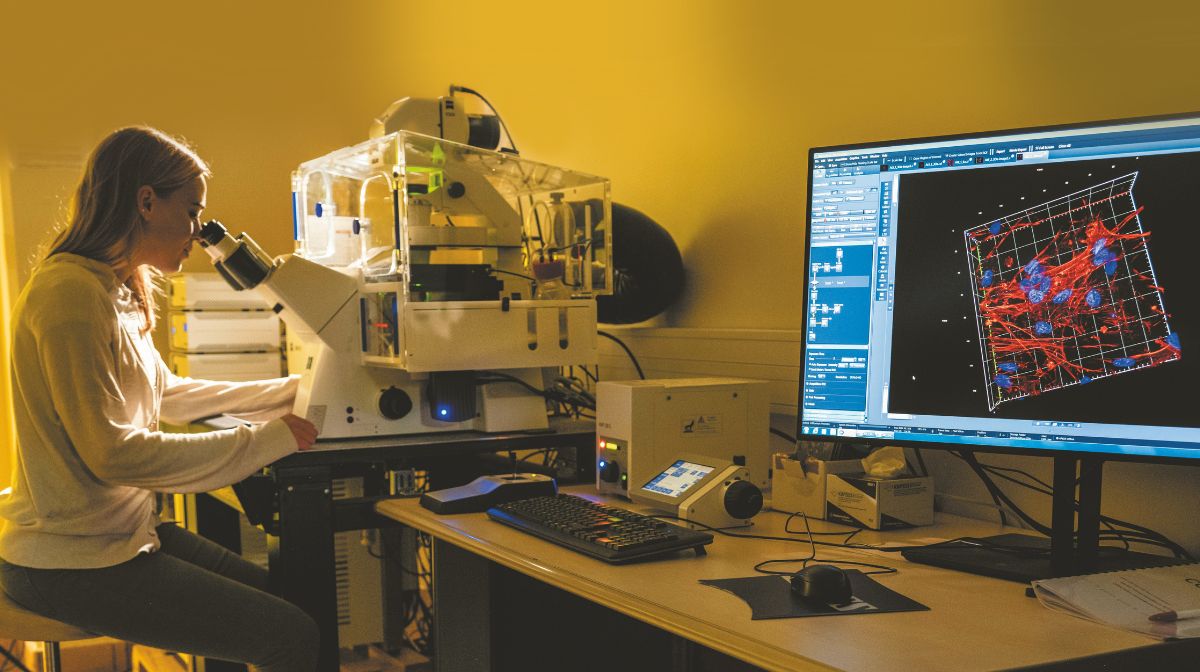
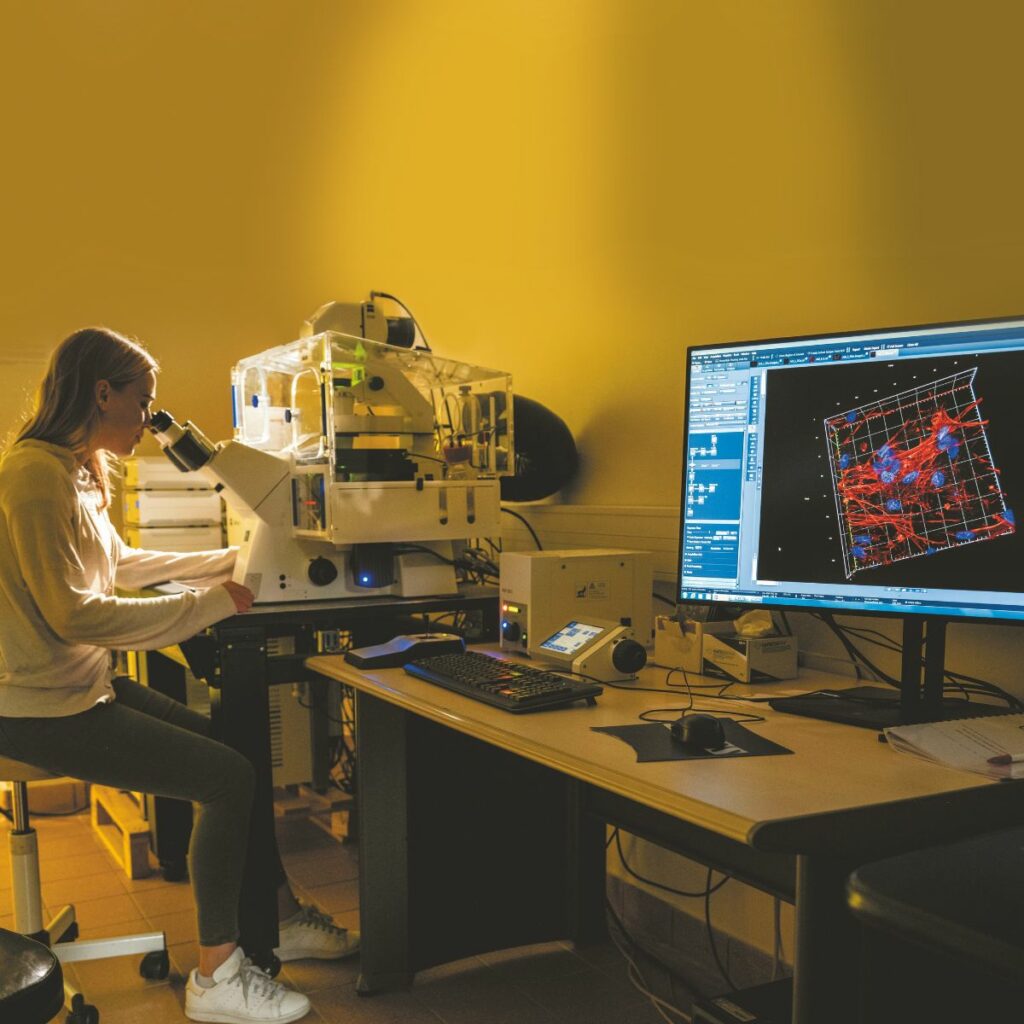
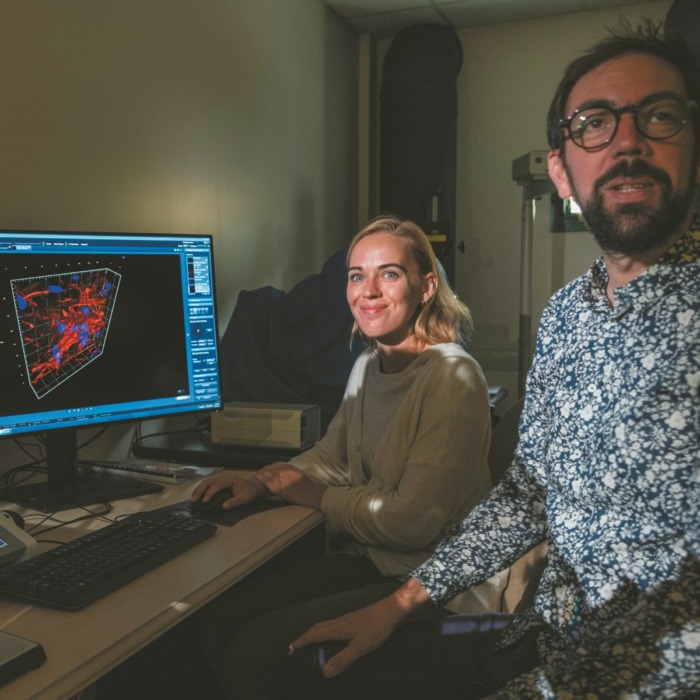
Once the skin cells are isolated, they are cultured and observed in real time on a computer in this robotic microscope.
The redder the cell nucleus, the more strongly the gene that codes for collagen is expressed. This is a sign that the cell anchored in the biomaterial is active and synthesizes new components of the skin.


Gwenaël Rolin places the culture fluid with the skin cells on the biomaterial. Are they well distributed throughout the material?
Here is the 3D visualization of a section of the biomaterial, eight days after cell seeding, created by Marion Tissot, laboratory technician. Each blue disc is a cell nucleus. Here we see that the skin cells are evenly distributed throughout the biomaterial. First test validated!

After biologically qualifying the product, we will measure its mechanical properties under the keen observation of Tiguida Kadiakhe, PhD student in Biomechanics at the CNRS FEMTO-ST Institute. The product must absolutely replicate the human dermis and be both flexible and resistant. The biomaterial is subjected to significant stresses to control its elasticity and measure all of its mechanical properties. It is important to allow it to stretch to accommodate the flexion of an ankle or knee and promote healing. The data is compared with that of human skin. Verdict? The elasticity is as expected!
The first human clinical trials are scheduled to begin in 2025. The product will initially be used in reconstructive surgery and chronic wounds, but could one day also be used to treat victims of severe burns.
A report prepared by Gwenaël Rolin’s team in the laboratory Host-graft-tumor interactions as well as cell and genetic engineering (Unit 1098 Inserm/EFS/Université de Franche-Comté) and in the Center for Clinical Research 1431 (CIC 1431 Inserm/CHRU Besançon/University of Franche-Comté).
The TissYou project benefits from European funding from Eurostars 2, of which the institute is a consortium member Rightthe Besançon University Hospital, the Rescoll company, the Straticell company (Belgium) and the Ludwig Boltzmann Research Institute (Austria).
Photos: Inserm/François Guénet
Author: LA
also read